Molecular Pathways Explain Why Long COVID Hits Women Harder
Gut leakiness and low testosterone linked to chronic fatigue in long COVID.

Research published today in Cell Reports Medicine reveals key biological differences that may explain why women with long COVID — especially those who develop chronic fatigue syndrome — tend to experience more severe and persistent symptoms than men do.
Post COVID-19 condition, or long COVID, is diagnosed when neurological, respiratory or gastrointestinal symptoms develop or continue three months or more after an acute SARS-CoV-2 infection.
The likelihood of developing long COVID is three times higher for women than men, but until now the underlying biological mechanisms driving this disparity have remained unknown.
The new research suggests potential targets for treatment that could bring relief to the 3.5 million Canadians who reported having had long COVID as of June 2023, according to Statistics Canada.
“We are focusing on a subset of patients with the most devastating symptoms that are very similar to chronic fatigue syndrome,” explains principal investigator Shokrollah Elahi, an immunology professor in the Mike Petryk School of Dentistry. “They didn't have these symptoms prior to COVID and most had only mild COVID-19 disease, so they were not hospitalized.”
Elahi’s team carried out blood and genetic tests on 78 patients with long COVID one year after their acute diagnosis, as well as a control group of 62 people who did not develop long COVID after infection with SARS-CoV-2.
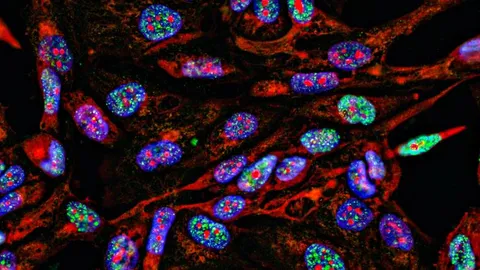
Through analysis of immune cells, biomarkers in the blood and RNA sequencing, they identified a distinct immune signature in female versus male patients.
They found evidence of “gut leakiness” in the women patients, including elevated blood levels of intestinal fatty acid binding protein, lipopolysaccharide, and the soluble protein CD14 — all signs of gut inflammation that can then trigger further systemic inflammation once they reach the circulatory system.
“This suggests that probably at the earliest stage of disease when patients get acute SARS-CoV-2 infection, there is a tendency that the females’ guts are more prone to viral infection,” Elahi says.
The team also found lower red blood cell production or anemia in the female patients. This suggests that elevated levels of inflammatory factors in females with long COVID adversely affect their blood production, Elahi says.
In addition, the researchers uncovered dysregulated sex hormones in the long COVID patients, finding reduced testosterone levels in affected women and decreased estrogen in male patients, as well as lower levels of the hormone cortisol in both.
The researchers reported that women with lower testosterone levels had higher levels of inflammation in their blood. Testosterone normally helps control inflammation, so reduced levels may make women more vulnerable to ongoing inflammatory responses, the researchers posit. Lower testosterone levels were also linked to symptoms such as brain fog, depression, pain and fatigue.
The findings suggest that hormone imbalances could play an important role in long COVID, particularly how it affects women, Elahi says.
These results are similar but not identical to what is found in idiopathic (of unknown cause) chronic fatigue syndrome, now referred to as myalgic encephalomyelitis/chronic fatigue syndrome or ME/CFS, which also disproportionately affects women. For example, anemia is not associated with chronic fatigue, but chronic inflammation is a characteristic.
The Elahi team’s findings are reinforced by another recent international study of more than 500 patients, which also reported anemia as a major biological underpinning of long COVID.
Elahi plans to further verify his findings by testing potential treatments in mice that have long COVID, and he is seeking funding for a clinical trial.
He proposes an individualized approach to treatment depending on each patient’s test results that might include anemia treatment, anti-inflammatory drugs and even sex hormones.
He also intends to continue exploring similarities between the neurological symptoms of long COVID and those associated with HIV infection.
Reference: Shahbaz S, Osman M, Syed H, et al. Integrated immune, hormonal, and transcriptomic profiling reveals sex-specific dysregulation in long COVID patients with ME/CFS. CR Med. 2025;0(0). doi: 10.1016/j.xcrm.2025.102449
This article has been republished from the following materials. Note: material may have been edited for length and content. For further information, please contact the cited source. Our press release publishing policy can be accessed here.